Study Questions
Introduction
Which client has the highest risk of developing a postoperative infection?
Explanation
The correct answer is choice A.A client with gestational diabetes mellitus has a higher risk of developing a postoperative infection after caesarean section because diabetes impairs wound healing and increases susceptibility to infection.
Choice B is wrong because active herpes virus infection does not increase the risk of surgical site infection after caesarean section.
Choice C is wrong because placenta previa is not a risk factor for postoperative infection after caesarean section.
Choice D is wrong because fetal breech presentation does not increase the risk of surgical site infection after caesarean section.
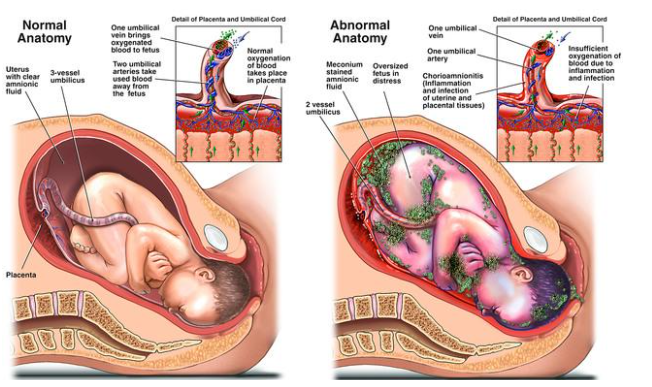
Some of the other risk factors for postoperative infection after caesarean section are high body mass index, intrapartum fever, prolonged rupture of membranes, prolonged labor, chorioamnionitis, anemia, and vertical skin incision.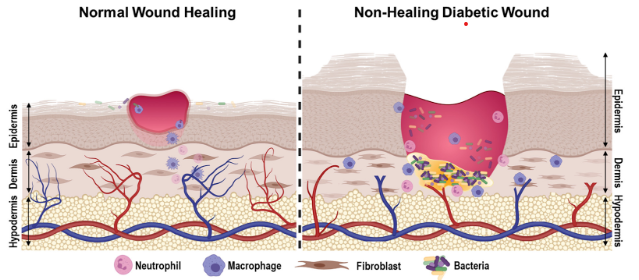
The nurse notices that the client has a large amount of bright red blood on her perineal pad.
What is the nurse’s priority action?.
Explanation
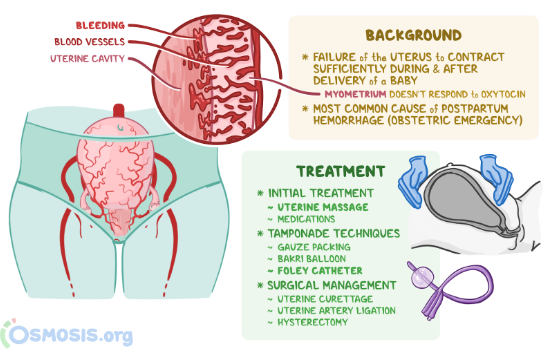
The correct answer is choice B. Massage the client’s fundus and check for firmness.This is because the most common cause of postpartum hemorrhage is uterine atony, which is a lack of contraction of the uterus after delivery.Massaging the fundus stimulates the uterus to contract and reduces bleeding from the placental site.Checking for firmness ensures that the uterus is not distended by blood clots or retained placental fragments, which can also cause hemorrhage.
Choice A is wrong because assessing the client’s vital signs and level of consciousness is not a priority action.
These are important indicators of blood loss and shock, but they do not address the source of bleeding.The nurse should first try to stop the bleeding by massaging the fundus and then assess the client’s status.
Choice C is wrong because notifying the provider and preparing for a blood transfusion are not priority actions.
These are interventions that may be needed if the bleeding does not stop with fundal massage or if the client develops signs of severe hemorrhage or shock.However, they are not the first steps to take in managing postpartum hemorrhage.
Choice D is wrong because administering oxytocin as prescribed to stimulate uterine contractions is not a priority action.Oxytocin is a uterotonic medication that can help prevent and treat postpartum hemorrhage by causing sustained uterine contractions.
However, it is not the first intervention to try in case of bleeding.The nurse should first massage the fundus and check for firmness, and then administer oxytocin if ordered by the provider.
Normal ranges for blood loss after delivery are less than 500 mL for vaginal birth and less than 1000 mL for cesarean birth.Normal ranges for vital signs and level of consciousness vary depending on the individual client, but some signs of hypovolemia and shock include tachycardia, hypotension, tachypnea, pallor, cold clammy skin, oliguria, anxiety, confusion, and loss of consciousness.Normal range for uterine firmness is a well-contracted uterus that feels like a hard ball at or below the umbilicus.
The nurse should include that which of the following conditions can lead to a caesarean delivery? (Select all that apply.)
Explanation
The correct answer is choice A, C, D and E. These are all conditions that can lead to a caesarean delivery.
Choice A is correct because cephalopelvic disproportion (CPD) means that the baby’s head or body is too large to fit through the mother’s pelvis.This can cause prolonged or obstructed labor and fetal distress.
Choice B is wrong because gestational hypertension (high blood pressure during pregnancy) is not a direct indication for a caesarean delivery.However, it can be associated with other complications such as preeclampsia, placental abruption or fetal growth restriction that might require a caesarean delivery.
Choice C is correct because fetal malposition means that the baby is not in the optimal position for vaginal delivery.
This includes breech (feet or buttocks first), transverse (sideways) or oblique (diagonal) presentations.These can increase the risk of cord prolapse, fetal injury or uterine rupture.
Choice D is correct because placenta abruption means that the placenta separates from the uterine wall before delivery.
This can cause severe bleeding, fetal hypoxia or stillbirth.A caesarean delivery is usually performed to save the mother and the baby.
Choice E is correct because cord prolapse means that the umbilical cord slips through the cervix ahead of the baby.
This can compress the cord and cut off the blood supply to the baby.A caesarean delivery is usually performed as an emergency to prevent fetal death.
The nurse should explain that which of the following types of anesthesia is most commonly used for this procedure?.
Explanation
The correct answer is choice B.Spinal anesthesia is the most commonly used type of anesthesia for caesarean delivery.It is administered around the spinal cord using a needle and it numbs the lower body for three to four hours.It has the advantages of being fast-acting, providing good operating conditions, and having minimal effects on the fetus.
Choice A is wrong because general anesthesia is rarely used for caesarean delivery unless there is an emergency or a contraindication for regional anesthesia.It involves putting the mother to sleep with drugs that can cross the placenta and affect the fetus.
Choice C is wrong because epidural anesthesia is not as commonly used as spinal anesthesia for caesarean delivery.It is administered around the nerves in the lower back and it requires a larger dose and a longer time to work than spinal anesthesia.
Choice D is wrong because local anesthesia is rarely used for caesarean delivery and only for minor procedures such as repairing a wound or removing stitches.It involves injecting a drug into the skin or tissue to numb a small area.
The nurse should identify that which of the following findings is a potential complication of this procedure?.
Explanation
The correct answer is choice A.Urinary output of 40 mL/hr is a potential complication of caesarean delivery because it indicates inadequate fluid intake, blood loss, or urinary tract injury.The normal range of urinary output is 30 to 60 mL/hr.
Choice B is wrong because incision site with serous drainage is a normal finding after caesarean delivery and does not indicate infection or bleeding.
Choice C is wrong because abdominal pain relieved by analgesics is also a normal finding after caesarean delivery and does not indicate any complication.
Choice D is wrong because uterus palpable at the umbilicus is an expected finding after caesarean delivery and indicates that the uterus is contracting and returning to its pre-pregnancy size.
What should the nurse assess?
Explanation
The correct answer is choice A. The patient’s allergies.
The nurse should assess the patient’s allergies before Caesarean delivery to prevent any adverse reactions to medications, anesthesia, or latex products that may be used during the procedure.
Allergies can cause serious complications such as anaphylaxis, which can be life-threatening for both the mother and the baby.
Choice B is wrong because the patient’s age is not a relevant factor for Caesarean delivery.
Age does not affect the surgical technique or the outcome of the operation.
Choice C is wrong because the patient’s height is not a relevant factor for Caesarean delivery.
Height does not affect the size of the incision or the amount of blood loss during the surgery.
Choice D is wrong because the patient’s weight is not a relevant factor for Caesarean delivery.
Weight does not affect the type of anesthesia or the risk of infection after the surgery.
Normal ranges for vital signs and laboratory values are not applicable for this question.
What should the nurse do to support the client emotionally?
Explanation
The correct answer is choice C. Address any concerns or anxieties the client may have regarding the procedure.Emotional support is a critical aspect of quality care throughout pregnancy and childbirth.Women who have a caesarean section may experience a range of emotions, such as depression, regret, or lower self-esteem.
The nurse should provide emotional support by listening to the client’s feelings, answering their questions, and reassuring them about the procedure.
Choice A is wrong because educating the client about the surgical procedure is not enough to support them emotionally.
The client may still have fears or worries that need to be addressed.
Choice B is wrong because administering prescribed medications as ordered by the healthcare provider is not directly related to emotional support.
Medications may help with pain relief or infection prevention, but they do not address the client’s psychological needs.
Choice D is wrong because ensuring that informed consent has been obtained from the client is a legal and ethical requirement, but it does not necessarily imply emotional support.
The client may still feel coerced, uninformed, or unhappy about the procedure.
What should the nurse pay special attention to?
Explanation
The correct answer is choice C. The patient’s abdomen and pelvic area.
The nurse should pay special attention to the patient’s abdomen and pelvic area before Caesarean delivery because this is where the surgery will take place.
The nurse should assess the size and position of the uterus, the fetal heart rate and movement, and any signs of infection or bleeding in the abdominal and pelvic area.
The nurse should also prepare the patient for the surgery by shaving the pubic hair, inserting a urinary catheter, and administering prophylactic antibiotics if ordered.
Choice A is wrong because the patient’s medical history is not as relevant as the current physical examination before Caesarean delivery.
The nurse should review the medical history for any risk factors or complications, but this is not the main focus of the examination.
Choice B is wrong because the patient’s allergies are not as important as the patient’s abdomen and pelvic area before Caesarean delivery.
The nurse should ask about any allergies to medications, latex, or iodine, but this is not the primary concern of the examination.
Choice D is wrong because the patient’s height is not as significant as the patient’s abdomen and pelvic area before Caesarean delivery.
The nurse should measure the patient’s height and weight to calculate the body mass index (BMI), but this is not the main objective of the examination.
What medication should the nurse administer?
Explanation
Prophylactic antibiotics and antacids are commonly given before a Caesarean delivery to prevent infection and reduce the risk of aspiration.Antibiotics can reduce the incidence of postoperative endometritis and wound infection.Antacids can neutralize the stomach acid and lower the pH, which can minimize the lung injury if aspiration occurs.
Choice B is wrong because painkillers and sedatives are not routinely given before a Caesarean delivery.Painkillers are usually given after the surgery or during the surgery if regional anesthesia is used.Sedatives are not recommended because they can cause respiratory depression and cross the placenta to affect the baby.
Choice C is wrong because antidepressants and antipsychotics are not indicated for a Caesarean delivery unless the woman has a psychiatric condition that requires them.These medications can have adverse effects on the mother and the baby, such as bleeding, hypertension, cardiac arrhythmias, sedation, withdrawal symptoms, and neurobehavioral changes.
Choice D is wrong because antihistamines and decongestants are not relevant for a Caesarean delivery.Antihistamines can cause sedation, dry mouth, and urinary retention, and decongestants can cause hypertension, tachycardia, and insomnia.These medications can also cross the placenta and affect the baby’s health.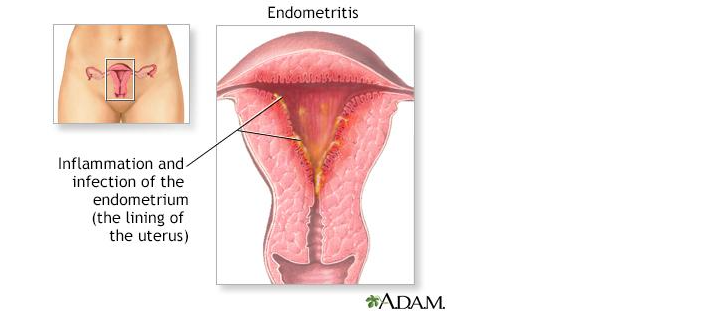
What should the nurse educate the patient about?
Explanation
The correct answer is choice D. All of the above.
The nurse should educate the patient about the risks, benefits and expected outcomes of Caesarean delivery before surgery.
Choice A is wrong because it is not enough to inform the patient only about the risks of surgery, such as infection, bleeding, injury to organs or anesthesia complications.
The patient also needs to know the benefits and expected outcomes of surgery.
Choice B is wrong because it is not enough to inform the patient only about the benefits of surgery, such as avoiding labor complications, delivering a healthy baby or having a planned date of birth.
The patient also needs to know the risks and expected outcomes of surgery.
Choice C is wrong because it is not enough to inform the patient only about the expected outcomes of surgery, such as the length of hospital stay, the recovery process or the wound care.
The patient also needs to know the risks and benefits of surgery.
Complications of Caesarean delivery
The nurse notices that the client has a fever of 38.2°C, increased redness and swelling at the incision site, and foul-smelling lochia.
What is the most likely cause of these findings?.
Explanation
The correct answer is choice A. Infection.The client’s fever, increased redness and swelling at the incision site, and foul-smelling lochia are all signs of infection, which is a common complication of cesarean delivery.
Choice B. Hemorrhage is wrong because hemorrhage would cause excessive bleeding, low blood pressure, and rapid pulse, which are not mentioned in the question.
Choice C. Deep vein thrombosis is wrong because deep vein thrombosis would cause pain, swelling, and tenderness in the legs, which are not mentioned in the question.
Choice D. Wound dehiscence is wrong because wound dehiscence would cause separation of the incision edges, drainage of serous fluid, and exposure of underlying tissues, which are not mentioned in the question.
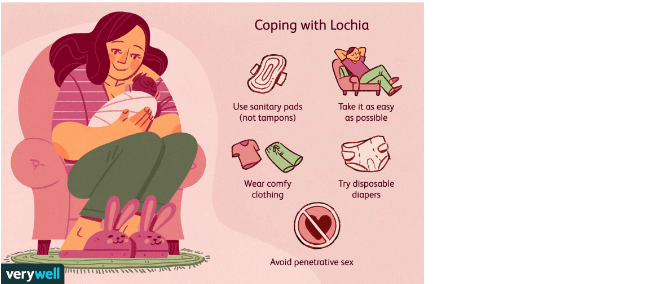
Normal ranges for lochia are as follows:
• Lochia rubra: bright red blood and clots that last for 3 to 4 days after delivery
• Lochia serosa: pinkish-brown discharge that lasts for 4 to 10 days after delivery
• Lochia alba: yellowish-white discharge that lasts for 10 to 14 days after delivery
Foul-smelling lochia indicates infection and should be reported to the health care provider.

The nurse observes that the client has soaked two perineal pads in one hour, has a heart rate of 120 beats per minute, and has a blood pressure of 90/60 mmHg.
What is the priority intervention for this client?.
Explanation
The correct answer is choice A. Apply pressure to the bleeding site.This is because the client is showing signs of postpartum hemorrhage (PPH), which is severe vaginal bleeding after childbirth.PPH can occur up to 12 weeks postpartum, but it is more common within the first 24 hours.PPH can be caused by uterine atony, retained placenta, or trauma to the reproductive organs.
Applying pressure to the bleeding site can help to control the blood loss and prevent shock.
Choice B. Encourage early ambulation is wrong because it can worsen the bleeding and increase the risk of fainting.Early ambulation is beneficial for preventing thromboembolism and promoting recovery, but it should be done after the bleeding is stabilized.
Choice C. Apply sterile dressings to the incision is wrong because it does not address the source of bleeding, which is likely from the vagina or uterus.The incision site may also bleed, but it is usually less than the vaginal bleeding.
Applying sterile dressings to the incision can help to prevent infection, but it is not a priority intervention for PPH.
Choice D. Encourage frequent voiding is wrong because it can cause bladder distension and interfere with uterine contraction.A full bladder can displace the uterus and prevent it from compressing the blood vessels where the placenta was attached.
Encouraging frequent voiding can help to maintain bladder function and reduce discomfort, but it is not a priority intervention for PPH.
Normal ranges for heart rate are 60-100 beats per minute and for blood pressure are 90/60-120/80 mmHg.Normal blood loss after cesarean delivery is less than 1000 mL.
Which of the following instructions should the nurse include? (Select all that apply.).
Explanation
The correct answer is choice A, B, C and D. These are all measures to prevent deep vein thrombosis (DVT) after caesarean delivery.DVT is a blood clot that forms in the deep veins of the legs or arms and can break off and travel to the lungs, causing a life-threatening condition called pulmonary embolism (PE).
Choice A is correct because wearing anti-embolism stockings as prescribed can help improve blood flow and reduce swelling in the legs.
Choice B is correct because avoiding crossing your legs when sitting or lying down can prevent pressure on the veins and reduce the risk of blood clots.
Choice C is correct because performing ankle and calf exercises every hour while awake can stimulate blood circulation and prevent blood from pooling in the lower extremities.
Choice D is correct because drinking at least 3 liters of fluid per day can help prevent dehydration, which can thicken the blood and increase the risk of clotting.
Choice E is wrong because elevating your legs above your heart level when resting can impair venous return and increase the risk of DVT.This position is recommended for patients with arterial insufficiency, not venous insufficiency.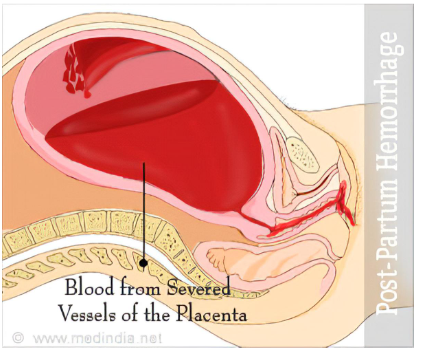
The nurse notices that the client’s incision site has opened and there is visible bowel protruding from the wound.
What is the appropriate action for the nurse to take?.
Explanation
The correct answer is choice B. Cover the wound with a sterile, moist dressing and notify the healthcare provider.
This is because the client has a wound dehiscence with evisceration, which is a serious complication that requires immediate medical attention.
The sterile, moist dressing will help prevent infection and keep the bowel tissue moist until surgery can be performed.
Choice A is wrong because pushing the bowel back into the abdomen can cause further damage and increase the risk of infection and peritonitis.
Choice C is wrong because irrigating the wound with normal saline and applying an antibiotic ointment can also introduce bacteria and irritate the bowel tissue.
Choice D is wrong because leaving the wound exposed to air can cause the bowel tissue to dry out and necrose, which can lead to sepsis and shock.
Which of the following findings should alert the nurse to this complication?.
Explanation
Answer and explanation..
The correct answer is choice D. All of the above.Urinary retention is a common complication after caesarean delivery, and it can be detected by measuring the postvoid residual bladder volume (PVRBV) with an ultrasound scan.A PVRBV of more than 150 mL is considered abnormal and indicative of urinary retention.
The following findings should alert the nurse to this complication:
• Inability to void within 6 hours after delivery: This is a sign of overt urinary retention, which occurs in about 7.4% of women who had a caesarean delivery.It may be caused by factors such as pain, anxiety, anesthesia, or bladder trauma.
• Distended bladder palpable above the symphysis pubis: This is a sign of covert urinary retention, which occurs in about 16.7% of women who had a caesarean delivery.It means that the bladder is overfilled but the woman does not feel the urge to void or has difficulty initiating micturition.
• Urinary output of less than 30 mL per hour: This is a sign of inadequate bladder emptying, which may lead to urinary tract infection, bladder damage, or renal impairment.It may be due to factors such as morphine-related postoperative analgesia, multiple pregnancy, or low body mass index, which are associated with increased risk of urinary retention after caesarean delivery.
Normal ranges for PVRBV and urinary output are:
• PVRBV: less than 150 mL
• Urinary output: more than 30 mL per hour
Patient Education
Which of the following statements by the client indicates an understanding of the teaching?.
Explanation
The correct answer is choice A.“I will avoid lifting anything heavier than my baby for the next 6 weeks.” This statement indicates that the client understands the importance of limiting physical activity and protecting the incision site from strain or injury.Lifting heavy objects can increase the risk of bleeding, infection, or wound dehiscence.
Choice B is wrong because resuming regular exercise routine as soon as getting home is not advisable after a C-section.The client should gradually increase activity levels and avoid strenuous exercises until cleared by the healthcare provider.
Choice C is wrong because ibuprofen may not be sufficient for pain relief after a C-section.The client may need stronger pain medications prescribed by the healthcare provider and should follow the instructions on how to take them safely.
Choice D is wrong because removing the dressing from the incision site tomorrow is too soon.The client should keep the incision site clean and dry and follow the healthcare provider’s instructions on when and how to change the dressing.Removing the dressing too early can increase the risk of infection or wound dehiscence.
Which of the following findings should alert the nurse to this complication?.
Explanation
The correct answer is choice A. Shortness of breath and chest pain are signs of pulmonary embolism (PE), which is a life-threatening complication of deep vein thrombosis (DVT).DVT is a type of blood clot that can occur in the legs or arms, especially during pregnancy and postpartum.PE happens when a blood clot breaks off and travels to the lungs, blocking blood flow.
Choice B is wrong because nausea and vomiting are not specific signs of thromboembolism.
They can be caused by many other conditions, such as morning sickness, food poisoning, or medication side effects.
Choice C is wrong because headache and blurred vision are not typical signs of thromboembolism.
They can be associated with other pregnancy complications, such as preeclampsia or eclampsia.
Choice D is wrong because fever and chills are not common signs of thromboembolism.
They can indicate an infection or inflammation, such as mastitis or endometritis.
Pregnant women have a higher risk of developing DVT and PE because of hormonal changes, increased blood clotting factors, reduced blood flow to the legs, and other factors.The risk is even higher after a caesarean delivery.
Therefore, it is important to know the signs and symptoms of thromboembolism and seek immediate medical attention if they occur.Thromboembolism can be prevented and treated with anticoagulant medications, compression stockings, and physical activity.
Which of the following behaviors by the client indicates effective bonding? (Select all that apply.).
Explanation
The correct answer is choices A, B, C and E. These behaviors by the client indicate effective bonding because they show affection, attention, communication and comfort to the newborn.
Holding the newborn close to her chest promotes skin-to-skin contact and warmth.
Making eye contact with the newborn fosters visual recognition and attachment.
Talking to the newborn in a soft voice stimulates auditory development and soothes the newborn.
Stroking the newborn’s hair and skin enhances tactile stimulation and bonding.
Choice D is wrong because handing the newborn to a family member when crying does not indicate effective bonding.
It shows that the client is unable or unwilling to cope with the newborn’s needs and emotions.
It may also interfere with the establishment of breastfeeding and maternal-infant attachment.
The client should try to calm the newborn by holding, rocking, feeding or changing him or her.
Which nursing intervention should be included in preoperative care?
Explanation
The correct answer is choice C) Encouraging coughing and deep breathing exercises.
This is because coughing and deep breathing exercises can help prevent atelectasis and pneumonia, which are common postoperative complications of C-section.
Coughing and deep breathing exercises also promote oxygenation and circulation.
Choice A) Administering an opioid analgesic is wrong because opioids can cause respiratory depression and sedation, which are not desirable before surgery.
Opioids can also cross the placenta and affect the fetus.
Choice B) Assessing for signs of deep vein thrombosis is wrong because this is not a priority intervention before surgery.
Deep vein thrombosis is more likely to occur after surgery due to immobility and venous stasis.
Choice D) Providing a high-carbohydrate meal is wrong because this can increase the risk of aspiration during surgery.
The client should be kept NPO (nothing by mouth) for at least 6 hours before surgery.
Explanation
The correct answer is choiceD) Use of incentive spirometry.Incentive spirometry is a device that helps patients take slow, deep breaths to expand their lungs and prevent respiratory complications such as pneumonia and atelectasis.Incentive spirometry also helps clear mucus and fluids from the lungs and improves ventilation.
Choice A is wrong because controlling anxiety and agitation may not directly prevent respiratory complications, although it may help patients breathe more comfortably.
Choice B is wrong because adequate nutrition and fluids are important for general health and recovery, but they do not specifically prevent respiratory complications.
Choice C is wrong because adequate pain control may help patients breathe more deeply and cough more effectively, but it is not enough to prevent respiratory complications by itself.
Choice E is wrong because early ambulation may improve blood circulation and reduce the risk of thromboembolism, but it does not directly prevent respiratory complications.
Explanation
The correct answer is choice A) Administering prophylactic antibiotics as ordered.According to the WHO guidelines for the prevention of surgical site infection (SSI), prophylactic antibiotics should be given within 60 minutes before skin incision and discontinued within 24 hours after surgery.
This reduces the risk of SSI by preventing bacterial colonization of the surgical site.
Choice B) Encouraging coughing and deep breathing exercises is wrong because this intervention is mainly for preventing respiratory complications, not SSI.Coughing and deep breathing exercises help to clear secretions and prevent atelectasis and pneumonia.
Choice C) Providing adequate pain control is wrong because this intervention is mainly for improving patient comfort and recovery, not SSI.Pain control may reduce stress and inflammation, but it does not directly affect the risk of SSI.
Choice D) Assessing for signs of deep vein thrombosis (DVT) is wrong because this intervention is mainly for preventing venous thromboembolism (VTE), not SSI.
DVT is a condition where a blood clot forms in a deep vein, usually in the legs.
It can cause pain, swelling, and redness.If the clot breaks off and travels to the lungs, it can cause a pulmonary embolism (PE), which can be life-threatening.
Some other intraoperative interventions for preventing SSI include using an alcohol-based skin prep, maintaining body temperature, using impervious wound protectors, and performing SSI surveillance.
Which of the following interventions should the nurse implement in the immediate postoperative period?
Explanation
The correct answer is choice D. All of the above interventions should be implemented in the immediate postoperative period after a caesarean delivery.
Choice A is correct because assessing the client’s fundus for firmness and position is important to prevent postpartum hemorrhage and monitor uterine involution.The fundus should be firm and at the level of the umbilicus one hour after delivery and descend into the pelvis at a rate of approximately 1 cm per day.
Choice B is correct because encouraging early ambulation can prevent thromboembolism, which is a potential complication of caesarean delivery.Early mobilization can also reduce pain, ileus, and urinary retention.
Choice C is correct because monitoring the client’s intake and output can help detect fluid imbalance, dehydration, or urinary tract infection.
Fluid intake should be adequate to maintain hydration and support lactation.Urinary output should be at least 30 mL per hour.
Therefore, choice D is correct because all of the above interventions are appropriate for postoperative care after a caesarean delivery.
Which of the following values should the nurse report to the provider?
Explanation
The correct answer is choice B. The client can use patient-controlled analgesia to self-administer opioids.This is a form of multimodal analgesia, which is the core principle for cesarean delivery pain management.
Patient-controlled analgesia allows the client to have control over their pain relief and adjust the dose according to their needs.
Choice A is wrong because the client may experience delays in receiving analgesics if they have to request them from the nurse, which can lead to inadequate pain relief and increased opioid consumption.
Choice C is wrong because ice packs are not recommended for cesarean delivery pain management, as they may interfere with wound healing and increase the risk of infection.
Choice D is wrong because deep breathing and relaxation exercises are not sufficient to manage acute postoperative pain, although they may be helpful as adjuncts to pharmacologic methods.
Which of the following findings should alert the nurse to a possible infection? (Select all that apply.).
Explanation
The correct answer is choice A and B.A temperature of 38°C (100.4°F) or higher and foul-smelling lochia or increased lochia are signs of infection after a C-section.A C-section is a major surgery that involves making incisions in the abdomen and uterus, which can get infected by bacteria.An infection can also affect the lining of the uterus (endometritis) or the urinary tract.
Choice C is wrong because tenderness or hardness in the lower abdomen is normal after a C-section and does not indicate an infection.
Choice D is wrong because a decreased white blood cell count is not a sign of infection.In fact, an increased white blood cell count is more likely to occur with an infection.
Choice E is wrong because increased thirst or dry mouth is not a sign of infection.It could be due to dehydration, medication, or hormonal changes.
Which of the following statements by the patient indicates an understanding of the teaching?
Explanation
“I can take ibuprofen or acetaminophen for pain relief.” This is because these are safe and effective medications for pain management after a C-section.
Choice A is wrong because driving is not recommended until the incision is healed and the pain is gone, which can take 4 to 6 weeks.
Choice B is wrong because lifting anything heavier than the baby can strain the incision and cause bleeding or infection.
Choice C is wrong because sexual intercourse should be avoided until the vaginal bleeding stops and the incision is healed, which can take 4 to 6 weeks or longer.
Which of the following behaviors by the patient indicates positive bonding?.
Explanation
The correct answer is choice A. Holding the baby close to her chest and stroking his hair indicates positive bonding between the mother and the newborn.This behavior shows that the mother is attentive, affectionate, and responsive to her baby’s needs.
Choice B is wrong because looking away from the baby and talking to the visitors suggests that the mother is not interested in or attached to her baby.She may be distracted, overwhelmed, or depressed.
Choice C is wrong because handing the baby to the nurse whenever he cries implies that the mother is not willing or able to comfort her baby.She may be avoiding contact or feeling helpless.
Choice D is wrong because feeding the baby with a bottle and avoiding eye contact indicates that the mother is not engaging with her baby.She may be missing an opportunity to bond through eye contact, touch, and voice.
The patient asks, “When will I be able to see my baby?” The health care team member is aware that promoting maternal bonding during the recovery period is especially important for postcesarean patients.
Why is this true?.
Explanation
The correct answer is choice B. Mothers may be at increased risk for poor bonding with the newborn.This is because cesarean delivery can interfere with the natural hormonal and physiological processes that facilitate maternal-infant attachment, such as skin-to-skin contact, breastfeeding initiation, and oxytocin release.Cesarean delivery can also cause more pain, stress, and anxiety for the mother, which can affect her emotional availability and responsiveness to the newborn.
Choice A is wrong because mothers do not necessarily have more problems with parenting skills after cesarean delivery.
Parenting skills depend on many factors, such as education, support, personality, and motivation.
Cesarean delivery may pose some challenges for postpartum recovery and care, but it does not imply that mothers are less competent or capable of parenting.
Choice C is wrong because mothers can breastfeed right away after cesarean delivery, unless there are medical contraindications or complications.
Breastfeeding is beneficial for both the mother and the newborn, as it provides nutrition, immunity, comfort, and bonding.However, breastfeeding after cesarean delivery may require more assistance and support from health care providers and family members, as well as alternative positions and techniques to avoid pain and discomfort.
Choice D is wrong because mothers do not necessarily resent the health care team member for keeping the newborn in the nursery.
Mothers may appreciate the help and care that the health care team member provides for them and their newborns.
However, keeping the newborn in the nursery may delay or reduce the opportunities for maternal-infant interaction and bonding.
Therefore, it is recommended to promote early and frequent contact between the mother and the newborn after cesarean delivery, as long as it is safe
Which information should be included in this report? (Select all that apply.)
Explanation
The correct answer is choices A, B, C and D. The type of anesthesia used, the estimated blood loss during surgery, the vital signs and oxygen saturation, and the allergies and medications given are all important information to be included in the hand-off report from the anesthesia provider to the recovery area staff.
These information help to assess the patient’s condition, monitor for complications, and plan for appropriate interventions.
Choice E is wrong because the Apgar scores of the newborn are not relevant to the patient’s recovery from cesarean delivery.
The Apgar scores are used to evaluate the newborn’s physical condition at birth and are usually reported by the neonatal team.
The recovery area staff should focus on the patient’s postoperative care and pain management.
Explanation
The correct answer is choiceD.A planned Caesarean section increases the rate of unexplained stillbirths at or after 34 weeks in future pregnancies.This is because a prior Caesarean section can cause placental abnormalities such as placenta previa and placenta accreta, which are associated with increased risk of stillbirth.
Choice A is wrong because the evidence comparing the risks of planned Caesarean section and vaginal delivery is mainly low or moderate quality.There are many confounding factors that can affect the outcomes of different modes of delivery, and most studies are observational and not randomized.
Choice B is wrong because the immediate maternal risks from a planned Caesarean section are not significantly higher than those of a planned vaginal delivery.However, a planned Caesarean section is associated with higher risks of infection, thromboembolism, wound complications, and longer hospital stay than a planned vaginal delivery.
Choice C is wrong because a vaginal birth is not associated with a comparable or higher maternal mortality rate than planned Caesarean section.The maternal mortality rate for planned Caesarean section is 0.01% and for planned vaginal delivery is 0.02%, which means there is no significant difference between the two modes of delivery.
Choice E is wrong because there is no evidence that an association exists between a prior Caesarean section and subsequent preterm birth, fetal growth restriction and spontaneous miscarriage.
These outcomes are more likely to be influenced by other factors such as maternal age, medical conditions,


